Reproductive medicine
Reproductive medicine is a branch of medicine concerning the male and female reproductive systems. It encompasses a variety of reproductive conditions, their prevention and assessment, as well as their subsequent treatment and prognosis.
Reproductive medicine has allowed the development of artificial reproductive techniques (ARTs) which have allowed advances in overcoming human infertility, as well as being used in agriculture and in wildlife conservation. Some examples of ARTs include IVF, artificial insemination (AI) and embryo transfer, as well as genome resource banking.
History
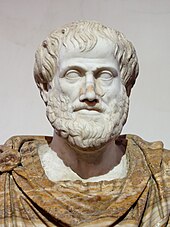
[edit]The study of reproductive medicine is thought to date back to Aristotle, where he came up with the “Haematogenous Reproduction Theory”.[1] However, evidence-based reproductive medicine is traceable back to the 1970s.[2] Since then, there have been many milestones for reproductive medicine, including the birth of Louise Brown, the first baby to be conceived through IVF in 1978.[3] Despite this, it was not until 1989 that it became a clinical discipline thanks to the work of Iain Chalmers in developing the systematic review and the Cochrane collection.[2]
Scope
[edit]Reproductive medicine addresses issues of sexual education, puberty, family planning, birth control, infertility, reproductive system disease (including sexually transmitted infections) and sexual dysfunction.[4] In women, reproductive medicine also covers menstruation, ovulation, pregnancy and menopause, as well as gynecologic disorders that affect fertility.[5]
The field cooperates with and overlaps mainly with reproductive endocrinology and infertility, sexual medicine and andrology, but also to some degree with gynecology, obstetrics, urology, genitourinary medicine, medical endocrinology, pediatric endocrinology, genetics, and psychiatry.
Conditions
[edit]Reproductive medicine deals with prevention, diagnosis and management of the following conditions. This section will give examples of a number of common conditions affecting the human reproductive system.
Infectious diseases
[edit]Reproductive tract infections (RTIs) are infections that affect the reproductive tract. There are three types of RTIs: endogenous RTIs, iatrogenic RTIs and sexually transmitted infections.[6] Endogenous RTIs are caused by an overgrowth of bacteria which is normally present. An example of an endogenous RTI is bacterial vaginosis.
Iatrogenic RTIs are infections contracted as a result of a medical procedure.
Sexually transmitted infections (STIs) are infections spread by sexual activity, usually by vaginal intercourse, anal sex, oral sex, and rarely manual sex. Many STIs are curable; however, some STIs such as HIV are incurable. STIs can be bacterial, viral or fungal and affect both men and women. Some examples of STIs are listed below:[7]
- Bacterial STIs
- Viral STIs
Cancer
[edit]Many parts of the Reproductive system can be affected by cancer. Below are some examples of Reproductive cancers:
Reproductive cancers affecting women
[edit]Reproductive cancers affecting men
[edit]A significant part of reproductive medicine involves promoting fertility in both men and women.
Causes of infertility or subfertility in women
[edit]- Ovulatory dysfunction
- Tubular dysfunction
- Pelvic inflammatory disease
- Endometriosis
- Previous sterilisation
- Previous surgery
- Cervical or uterine dysfunction
- Congenital abnormalities
- Fibroids
- Asherman's syndrome
- Hormonal issues
Causes of infertility or subfertility in men
[edit]- Problems with sperm number or function
- Tubular dysfunction
- Congenital abnormalities
- Prior sexually transmitted infections
- Vasectomy
- Problems with sperm delivery
- Premature ejaculation
- Damage to the reproductive organs
- Retrograde ejaculation
- Certain genetic diseases
Disorders of sex development
[edit]Congenital abnormalities
[edit]- Cervical abnormalities
- Cervical agenesis
- Cervical duplication
- Hymen abnormalities
- Uterine abnormalities
- Vaginal abnormalities
- Vulvar abnormalities
Disorders due to hormone excess
[edit]- Polycystic ovarian syndrome (PCOS)
- Granulosa cell tumour
- Leydig cell tumour
- Teratoma
Disorders due to hormone deficiency
[edit]Disorders due to hormone hypersensitivity
[edit]Disorders due to hormone resistance
[edit]Non-functioning endocrine tumours
[edit]- Ovarian cysts
- Carcinoma
- Teratoma
- Seminoma
Secondary endocrine disorders (originating in the pituitary gland)
[edit]Assessment and treatment
[edit]Assessment and treatment of reproductive conditions is a key area of reproductive medicine.
Female assessment starts with a full medical history (anamnesis) which provides details of the woman's general health, sexual history and relevant family history.[12] A physical examination will also take place to identify abnormalities such as hirsutism, abdominal masses, infection, cysts or fibroids. A blood test can inform the clinician of the endocrine status of the patient. Progesterone levels are measured to check for ovulation, and other ovulatory hormones can also be measured. Imaging techniques such as pelvic ultrasounds can also be used to assess the internal anatomy.[13]
Male assessment also starts with a history and physical examination to look for any visible abnormalities. Investigations of semen samples also take place to assess the volume, motility and number of sperm, as well as identifying infections.[14]
Once the investigations are complete, treatment of identified conditions can occur. For fertility issues, this may involve assisted reproductive technology (ART) such as in-vitro fertilisation (IVF) or fertility medication. There are surgical methods that can be used as treatment however these are now performed less frequently due to the increasing success of the less invasive techniques.[13] Treatment is also required for sexually transmitted infections (STIs). These can take the form of antibiotics for bacterial infections such as chlamydia[15] or highly active anti-retroviral therapy (HAART) for the HIV virus.[16]
Education and training
[edit]Before starting a career in reproductive medicine, individuals must first obtain an undergraduate degree. The next step is medical school, where they earn a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree. Specialists in reproductive medicine usually undergo medical residency training in obstetrics and gynecology followed by medical fellowship training in reproductive endocrinology and infertility. An alternative path to practicing reproductive medicine after medical school involves a medical residency in urology, followed by a medical fellowship in male infertility. The education and training required to practice reproductive medicine is typically 15-16 years in duration.[17][18][19] After completing medical fellowship, physicians can obtain board certification and must maintain continuing medical education (CME).[20] CME is necessary in reproductive medicine as advancements in technology and treatment options require ongoing learning and skill development.
For reproductive medicine specialists in contraception, other methods of training are possible. Specialists tend to be organized in specialty organizations such as the American Society for Reproductive Medicine (ASRM) and European Society of Human Reproduction and Embryology (ESHRE).
Anamnesis
[edit]The anamnesis or medical history taking of issues related to reproductive or sexual medicine may be inhibited by a person's reluctance to disclose intimate or uncomfortable information. Even if such an issue is on the person's mind, they often do not start talking about such an issue without the physician initiating the subject by a specific question about sexual or reproductive health.[21] Some familiarity with the doctor generally makes it easier for person to talk about intimate issues such as sexual subjects, but for some people, a very high degree of familiarity may make the person reluctant to reveal such intimate issues.[21] When visiting a health provider about sexual issues, having both partners of a couple present is often necessary, and is typically a good thing, but may also prevent the disclosure of certain subjects, and, according to one report, increases the stress level.[21]
Ethical and medicolegal issues
[edit]There are many ethical and legal issues surrounding reproductive medicine. In the UK the Human Fertilisation and Embryology Authority (HEFA) regulates many aspects of reproductive medicine in the UK, including IVF, Artificial Insemination, storage of reproductive tissue and research in this field. HEFA was established due to the Human Fertilisation and Embryology Act (1990). This act was reviewed and the Human Fertilisation and Embryology Act (2008) was passed through parliament as an update to the 1990 act.
For therapies such as IVF, many countries have strict guidelines. In the UK, referrals are only given to women under 40 who have either undergone 12 cycles of artificial insemination, or have tried and failed to conceive for 2 years.[22] While NICE recommends NHS clinical commissioning groups (CCGs) to provide 3 NHS funded cycles of IVF, many only offer 1 cycle, with some only offering IVF in exceptional circumstances on the NHS. If an individual does not meet the criteria or has gone through the maximum number of NHS-funded cycles, the individual will have to pay for private treatment[23]
Many reproductive technologies are seen to have ethical problems, including IVF, mitochondrial replacement therapy, germline modification, preimplantation genetic diagnosis.
There are many groups around the world which oppose to ARTs, including religious groups and pro-life charities such as LIFE.
References
[edit]- ^ Kremer, J. (2003-12-20). "The haematogenous reproduction theory of Aristotle". Nederlands Tijdschrift voor Geneeskunde. 147 (51): 2529–2535. ISSN 0028-2162. PMID 14735853.
- ^ a b Johnson, Martin H. (March 2013). "The early history of evidence-based reproductive medicine". Reproductive Biomedicine Online. 26 (3): 201–209. doi:10.1016/j.rbmo.2012.11.010. ISSN 1472-6491. PMID 23273757.
- ^ Clarke, Gary N. (July 2006). "A.R.T. and history, 1678-1978". Human Reproduction (Oxford, England). 21 (7): 1645–1650. doi:10.1093/humrep/del067. ISSN 0268-1161. PMID 16606642.
- ^ "KKIVF Centre". KK Women's and Children's Hospital. SingHealth. Retrieved 4 December 2015.
- ^ "Fertility and Reproductive Medicine". Washington University Physicians. Barnes-Jewish Hospital and St. Louis Children's Hospital. Retrieved 4 December 2015.
- ^ "Sexually Transmitted Diseases". www.fhi360.org. Retrieved 2019-09-25.
- ^ Scott, G.R. (2014). 'Sexually transmitted infections', in Walker, B.R. (ed.) Davidson's Principles & Practices of Medicine. Edinburgh: Elsevier, pp. 411-426
- ^ Strachan, M.W.J., Newell-Price, J. (2014). 'Endocrine disease', in Walker, B.R. (ed.) Davidson's Principles & Practices of Medicine. Edinburgh: Elsevier, pp. 760
- ^ "Center for Congenital Anomalies of The Reproductive Tract | Conditions We Treat | Boston Children's Hospital". www.childrenshospital.org. Retrieved 2019-09-25.
- ^ "Congenital Anomalies of the Bladder and Genitalia". Cleveland Clinic. Retrieved 2019-09-25.
- ^ Strachan, M.W.J., Newell-Price, J. (2014). 'Endocrine disease', in Walker, B.R. (ed.) Davidson's Principles & Practices of Medicine. Edinburgh: Elsevier, pp. 758
- ^ "Initial assessment of infertility". NICE. Retrieved 2019-09-25.
- ^ a b "Female infertility - Diagnosis and treatment - Mayo Clinic". www.mayoclinic.org. Retrieved 2019-09-25.
- ^ "Male infertility - Diagnosis and treatment - Mayo Clinic". www.mayoclinic.org. Retrieved 2019-09-25.
- ^ "Chlamydia Infections". medlineplus.gov. Retrieved 2019-09-25.
- ^ "Antiretroviral therapy for HIV infection in adults and adolescents". WHO.
- ^ American Medical Association (May 22, 2024). "Pre-med frequently asked questions". Retrieved September 11, 2024.
- ^ Washington University School of Medicine St. Louis. "Obstetrics and Gynecology, Overview of the Specialty". Retrieved September 11, 2024.
- ^ NYU Grossman School of Medicine. "Reproductive Endocrinology & Infertility Fellowship". Retrieved September 11, 2024.
- ^ "Reproductive Endocrinology and Infertility Certifying Exam". The American Board of Obstetrics & Gynecology. Retrieved September 11, 2024.
- ^ a b c 'The Cringe Report' By Susan Quilliam. Posted: 06/28/2011; J Fam Plann Reprod Health Care. 2011;37(2):110-112.
- ^ "Recommendations | Fertility problems: assessment and treatment | Guidance | NICE". www.nice.org.uk. 20 February 2013. Retrieved 2019-09-25.
- ^ "IVF - Availability". nhs.uk. 2017-10-20. Retrieved 2019-09-25.
Literature
[edit]- Lipshultz LI, Khera M, Atwal DT. Urology and the Primary Care Practitioner. Philadelphia: Elsevier, 2008.
- Naomi Pfeffer: The Stork and the Syringe: A Political History of Reproductive Medicine (Feminist Perspectives) Polity Press 1993, ISBN 0-7456-1187-7
- Speroff L, Glass RH, Kase NG. Clinical Gynecologic Endocrinology and Infertility. Fifth Edition. Williams and Wilkins, Baltimore MD, 1994 ISBN 0-683-07899-2
